Hypertension
Hypertension
The Blood Pressure is the force of blood traveling through and pushing outwards against your arteries. Hypertension, also known as HTN or High Blood Pressure, is a medical condition in which the blood pressure is chronically elevated. Hypertension or High Blood Pressure is the most common “chronic disease” worldwide. While Hypertension is a serious condition, you can manage it with a combination of lifestyle modifications and drug therapy. It starts with learning how to accurately measure your blood pressure…
MY BLOOD PRESSURE EDUCATION:
-
PAPER GUIDE – HOW TO CHECK MY BLOOD PRESSURE – Download ONE PAGE
-
PAPER GUIDE – MY BLOOD PRESSURE LOG – Download
-
VIDEO GUIDE – HOW TO CHECK MY BLOOD PRESSURE – Watch YouTube
-
HYPERTENSION – COMPREHENSIVE EDUCATION BOOKLET – Download
-
Understanding Hypertension – a simple brochure for patients – Download

For Hypertension Providers
-
JNC VII , JNC VII Express Card → JNC VIII
-
DASH (Dietary Approaches to Stop Hypertension)
-
Increased Creatinine with ACE-I or ARB – WHAT TO DO?
-
Hypertension SIMPLIFIED LONG (40 minutes) YOUTUBE VIDEO
-
The KDIGO 2021 Blood Pressure in CKD Guidelines
-
Good sleep guidelines
-
Magnesium benefits and Hypertension.. the underestimated mineral
-
Tell your patients to track their Blood Pressure – YouTube Video
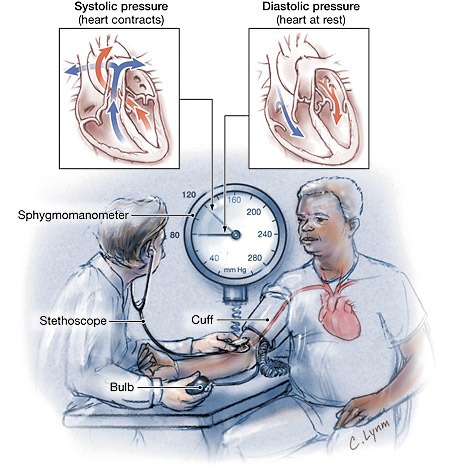
Blood pressure is the force of blood that is exerted against the walls of the arteries as the heart pumps blood throughout the body
HYPERTENSION
HYPERTENSION, also known as HTN or high blood pressure, is a medical condition characterized by chronically elevated blood pressure. This condition is quite common, with one in three American adults diagnosed with hypertension and one fourth of remaining adults having prehypertension. Prehypertension is not a distinct disease category, but rather a label used to identify individuals who are at high risk of developing hypertension. Currently, there are more than 80 million Americans and one billion people worldwide with hypertension.
This condition can be classified as either essential (primary) or secondary. Essential hypertension is responsible for 90% of all new cases and has no specific medical cause. On the other hand, secondary hypertension is a result of another medical condition, such as chronic kidney disease, that results in high blood pressure.
Persistent hypertension is a significant risk factor for a variety of health conditions, including strokes, heart attacks, congestive heart failure, chronic kidney disease, and dementia. Furthermore, it is the number one modifiable risk factor for approximately 12% of all deaths worldwide. In fact, even a moderate elevation of arterial blood pressure is known to reduce life expectancy.
Hypertension is typically diagnosed when an individual consistently has a systolic blood pressure of 140 mmHg or greater (the top number) and/or a diastolic blood pressure of 90 mmHg or greater (the lower number). In 2014, the Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure defined a blood pressure of 120/80 or less as the normal range, while blood pressure readings of 120/80 mmHg to 139/89 mmHg were classified as prehypertension. Individuals in this group may be able to manage their blood pressure through lifestyle modifications.
For patients with diabetes mellitus and almost all forms of kidney disease, studies suggest that blood pressure over 130/80 mmHg should be considered high and requires further treatment. Moreover, individuals with kidney disease who have more than one gram of protein in a 24-hour urine sample should aim for a blood pressure of 125/75 or lower.
Hypertension is classified as resistant or refractory only when blood pressure remains above the target level despite the use of three or more different antihypertensive medications at maximum dose, one of which must be a diuretic.
Risk Factors of ESSENTIAL or PRIMARY HYPERTENSION
Although lacking a specific medical cause, often has several contributing factors. These factors may include obesity, salt sensitivity, insulin resistance, genetics, lack of physical activity, and age.
- Obesity
Obesity is a significant risk factor for hypertension, with the risk being five times higher in individuals who are obese compared to those of normal weight. In fact, up to two-thirds of hypertension cases can be attributed to excess weight, and more than 85% of cases occur in individuals with a BMI greater than 25.
- Sodium or salt sensitivity
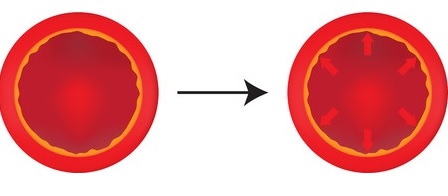
Sodium, which is the main component of table salt, is an environmental factor that has received significant attention with regards to hypertension. Approximately one-third of the essential hypertensive population is responsive to sodium intake. This is because increasing amounts of salt in a person’s bloodstream causes cells to release water (due to osmotic pressure) to balance the concentration gradient of salt between the cells and the bloodstream. This increases the pressure against the blood vessel walls, which can lead to a rise in the measured pressure inside the blood vessels. It’s worth noting that both sea salt and Kosher salt are similar to table salt in terms of their sodium content and their potential contribution to hypertension.
- Insulin resistance
The primary function of insulin is to regulate the levels of glucose in the body. However, insulin also has vasodilating properties. In individuals with normal blood pressure, insulin may stimulate sympathetic activity without increasing arterial pressure. However, in more severe conditions such as metabolic syndrome, the increased sympathetic activity may override the vasodilating effects of insulin. Insulin resistance, syndrome X, metabolic syndrome, dysmetabolic syndrome X, and hyperinsulinemia are interchangeable terms that have been suggested to be responsible for increased arterial pressure in some patients with hypertension. This feature is now widely recognized as a component of metabolic syndrome.
- Sleep apnea
Sleep apnea is a frequently overlooked cause of hypertension. It can often be effectively managed through weight loss and the use of nocturnal continuous positive airway pressure (CPAP), although other treatments such as the Mandibular Advancement Splint (MAS), Uvulopalatopharyngoplasty (UPPP or UP3), tonsillectomy, and/or adenoidectomy may also be beneficial. Sleep plays an important role in the regulation of blood pressure, and sleep disorders such as sleep apnea have been linked to hypertension. Sleep apnea is a condition in which a person’s breathing is interrupted during sleep, leading to repeated episodes of hypoxia (low oxygen levels) and hypercapnia (high carbon dioxide levels). These episodes can trigger a cascade of physiological responses that increase blood pressure, including the activation of the sympathetic nervous system and the renin-angiotensin-aldosterone system.
- Genetics (race and gender)
While hypertension is more common in younger men than women, the reverse is true for individuals over the age of 60. Hypertension is a complex disorder with a heritability of approximately 30%. To date, more than 50 genes have been examined in genetic association studies of hypertension, and new genes are continually being identified.
- Age
As people age, their blood vessels become less elastic, resulting in a smaller cross-sectional area during systole and an overall increase in mean arterial blood pressure.
- Inactivity
Lack of physical activity is a well-established risk factor for hypertension. Engaging in regular physical activity helps to lower blood pressure, improve overall cardiovascular health, and reduce the risk of developing other health problems associated with hypertension, such as heart disease and stroke.
Symptoms and Signs
Hypertension is typically detected incidentally during routine checkups by healthcare professionals. As a result, it can go undiagnosed for many years, earning it the name of a “silent disease.” Blood pressure measurement is the only way to test for hypertension. In most cases, hypertension does not have any symptoms, although some individuals may experience headaches, fatigue, dizziness, blurred vision, nosebleeds, frequent urination, facial flushing, transient insomnia, or difficulty sleeping due to feeling hot or flushed, tinnitus (ringing in the ears), muscle cramps, excessive sweating, or palpitations (irregular or rapid heartbeat).
Complications of Hypertension
Although elevated blood pressure alone is not considered an illness, it often necessitates treatment due to its short- and long-term effects on various organs, referred to as end-organ damage. The higher the blood pressure, the greater the risk of end-organ damage. Furthermore, high blood pressure raises the risk of several conditions, including
- Strokes or Cerebrovascular accident (CVA), transient ischemic attacks (TIA).
- Myocardial infarction (heart attack).
- Hypertensive cardiomyopathy (heart failure resulting from chronically elevated or high blood pressure).
- Hypertensive retinopathy (damage to the retina).
- Hypertensive nephropathy (chronic renal failure due to chronically elevated blood pressure or chronic kidney disease, CKD).
- Vascular dementia.
.
Diagnosis of HYPERTENSION
The diagnosis of hypertension is typically established based on consistently high blood pressure readings. This typically involves three or more measurements taken at least a week apart. However, in some cases, if the elevation is severe or if there is evidence of end-organ damage, the diagnosis may be made immediately and treatment initiated.
During the evaluation for hypertension, it is important for the patient to avoid adrenergic stimulants, such as those commonly found in cold medications (especially decongestants labeled with a D), as they can increase blood pressure and make it challenging to accurately diagnose hypertension. Similarly, the patient should refrain from taking non-steroidal anti-inflammatory agents (NSAIDs) or arthritis medications like Ibuprofen, as these medications can also raise blood pressure.
Home blood pressure monitoring can be a useful tool to measure blood pressure at various times of the day and in different settings, including at home and work. It can aid in the diagnosis of high or low blood pressure, and help monitor the effectiveness of medication or lifestyle changes aimed at controlling or reducing blood pressure levels.
Home blood pressure monitoring is a valuable tool for detecting white coat hypertension, which refers to an increase in blood pressure due to anxiety in a clinical setting. By tracking blood pressure measurements at home, patients can obtain a more accurate assessment of their true blood pressure levels and provide their healthcare providers with a record of their measurements over time. In addition, 24-hour ambulatory blood pressure monitoring using a specialized device can help to provide a more precise diagnosis of hypertension.
Tests performed in newly diagnosed Hypertension
Tests are carried out to identify potential causes of secondary hypertension and to look for signs of end-organ damage to the heart, eyes (retina), and kidneys. In addition, diabetes and elevated blood cholesterol levels, which are additional risk factors for developing cardiovascular disease, are also tested for and require management. Blood tests that are commonly performed include:
- Creatinine: This test is used to assess kidney function and to identify underlying renal disease as a cause of hypertension. It can also help monitor the possible side-effects of certain antihypertensive drugs.
- Urine samples are also collected to check for the presence of protein and/or microalbumin, as these can indicate underlying kidney disease or evidence of hypertensive renal damage.
- Electrolytes (sodium, potassium, calcium, and magnesium): These tests help to evaluate the balance of these minerals in the blood, which can affect blood pressure.
- Fasting blood glucose and Hemoglobin A1c: This test helps to identify the possibility of diabetes, which is a risk factor for hypertension.
- Fasting lipid profile: This test measures cholesterol and triglyceride levels in the blood, which are also risk factors for cardiovascular disease.
- Thyroid function tests: These tests help to evaluate the function of the thyroid gland, which can affect blood pressure.
- Serum uric acid: This test measures the level of uric acid in the blood, which can be elevated in some cases of hypertension.
Additional tests may include:
Additional tests that are often performed include an electrocardiogram (ECG) to assess the heart’s activity and identify any signs of strain due to high blood pressure, such as thickening of the heart muscle (known as left ventricular hypertrophy or LVH), which can increase the risk of fatal cardiovascular events. The ECG can also detect any abnormalities that may indicate previous silent cardiac events.
Another common test is an ultrasound of the kidneys to assess their structure and function and detect any abnormalities or damage due to hypertension.
To diagnose sleep apnea and evaluate its impact on blood pressure, a sleep study, also known as a polysomnogram, may be recommended. During this test, the patient spends the night in a sleep laboratory, where a variety of sensors are used to monitor their breathing, heart rate, brain waves, and other physiological parameters.
TREATMENT OF HYPERTENSION
- Lifestyle modification (non-pharmacologic treatment)
- The initial steps to manage mild to moderate hypertension involve weight reduction and regular aerobic exercise, such as jogging or swimming. These measures improve blood flow and help reduce the resting heart rate and blood pressure. While effective in lowering blood pressure, drug therapy is still necessary for many patients with moderate or severe hypertension to achieve a safe blood pressure level.
- Reducing the intake of dietary refined sugars and carbohydrates is recommended.
- Reducing sodium (salt) in the diet, which can decrease blood pressure in around 60% of people. Some individuals choose to use a salt substitute to lower their salt intake, but it is important to inform a healthcare provider if using a salt substitute because it may contain potassium chloride.
- Dietary change that can help reduce blood pressure is the DASH diet (Dietary Approaches to Stop Hypertension), which emphasizes fruits, vegetables, and low-fat or fat-free dairy foods. Research sponsored by the US National Institutes of Health shows that this diet is effective. Increasing daily calcium and magnesium can also boost dietary potassium, which can counteract the effect of sodium and reduce blood pressure, proving highly effective in hypertension management.
- Cessation of tobacco use and alcohol consumption have been found to lower blood pressure. Although the exact mechanisms are not fully understood, consumption of alcohol and nicotine leads to a temporary increase in blood pressure, especially systolic blood pressure. Abstaining from cigarette smoking is particularly important for individuals with hypertension because it reduces the risk of adverse outcomes such as stroke and heart attack. It is worth noting that coffee drinking or caffeine ingestion may cause a temporary increase in blood pressure, but it does not lead to chronic hypertension.
- Reducing stress can be an effective way to manage hypertension. Relaxation therapy, meditation, and other mind-body relaxation techniques can help to reduce stress levels. Additionally, reducing environmental stressors such as high sound levels and over illumination can also be beneficial. By reducing stress, blood pressure can be lowered and hypertension can be better managed.
Pharmacologic treatment of hypertension with medications
Unless hypertension is severe, it is strongly recommended to make lifestyle modifications, such as those discussed earlier, before starting drug therapy. For example, adopting the DASH diet has been repeatedly shown to effectively lower mildly-elevated blood pressure. If hypertension is severe enough to require immediate medication, lifestyle changes are initiated alongside drug therapy. The goal of treatment is to control blood pressure to less than 130/80 mmHg for most patients, and lower in certain cases, such as individuals with diabetes or kidney disease (some medical professionals recommend keeping levels less than 125/75 mmHg). Since each drug may reduce systolic blood pressure by 5–10 mmHg, multiple drugs are often necessary to achieve blood pressure control.
P.O. Box 1750
Lynn Haven, FL 32444 – 5950
United States of America
e-mail: info@TheVirtualNephrologist.com
tel : +1 (929) 379.6953
fax: +1 (850) 914.3004